Pretibial Myxedema, Nodular Variant: Unique Presentation and Clinical Course
Juniper Publishers- JOJ Dermatology & Cosmetics
Abstract
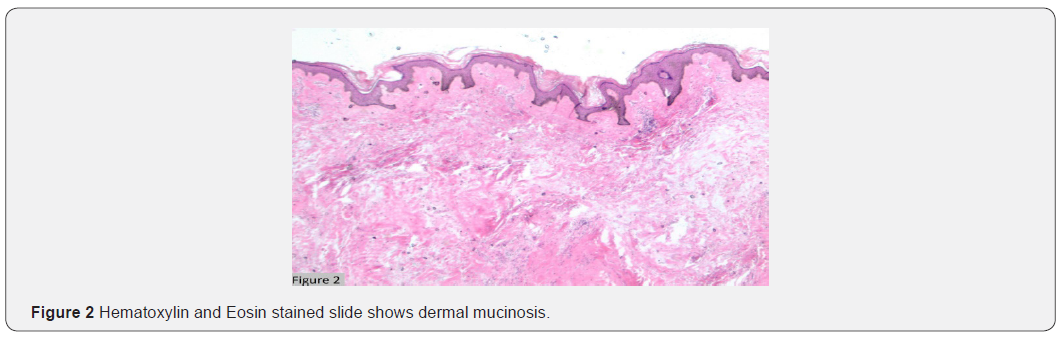
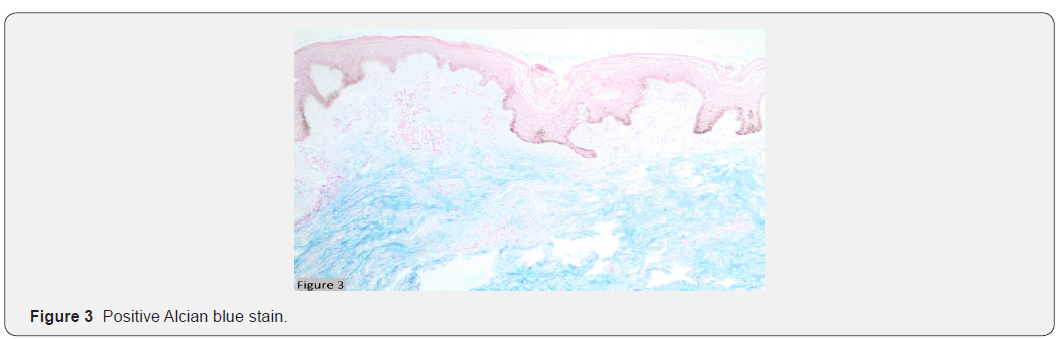
Literature has shown morphological diversity in the presentation and occurrence of pretibial myxedema following I-131 treatment. We present a case of a 47 y.o African American male with post I-131 hypothyroidism for Graves disease that presented with enlarging bilateral lower extremity and ankle lesions. Examination revealed firm, tender, hemispherical, large, hyperpigmented nodules. Ultrasound demonstrated nonspecific hypovascular nodular thickening of the skin. Excisional biopsy showed reactive dermal and subcutaneous fibrosis with dermal mucinosis. Alcian blue stain confirmed the diagnosis. Graves’ dermopathy is generally rare, with the nodular variant accounting for 10% of cases. Our case reflects a variable appearance of post-I-131 treatment dermopathy partially resistant to the multimodal treatment.
Keywords: Myxedema; Nodular Variant; Hypothyroidism; Dermopathy
Abbreviations: Radioactive iodine (I-131)
Introduction
Graves dermopathy is a rare entity (approximately 4%), with the nodular variant accounting for 10% of all reported cases [1]. Many patients with Graves’ disease receive radioactive iodine (I- 131) as a treatment. Literature has shown morphological diversity in the presentation and occurrence of pretibial myxedema following I-131 for Graves’ disease [2].
Case Report
A 47 year-old African American male presented with complaints of bilateral lower extremity and ankle lesions that developed after receiving radioactive ablation 20 years ago for his Graves’ disease. The lesions were causing constant discomfort and preventing him from wearing shoes. Examination revealed bilateral large firm, tender, hemispherical and hyperpigmented nodules at the distal portion of his lower extremities and ankles (Figure 1). Other findings include mild edema and Graves’ opthalmopathy. His lab tests revealed elevated thyrotropin-stimulating hormone levels at 15.94 mIU/mL and suppressed free thyroxine (T4) levels at 0.69 ng/dL consistent with his history of noncompliance. A previous ultrasound on the lesions showed nonspecific findings of hypovascular areas of diffuse nodular dermal soft tissue thickening involving both ankles. A decision to preform an extensive excisional biopsy of his left ankle lesions with skin grafting was made. Microscopically, the lesion showed reactive dermal and subcutaneous fibrosis with dermal mucinosis (Figure 2). A positive Alcian blue stain confirmed the diagnosis of pretibial myxedema (Figure 3). The excision measured 17x 7 cm.
Discussion
Pretibial myxedema, or thyroid dermopathy, is an infiltrative dermopathy occurring as a result of excess glycosaminoglycan deposition in the dermis and subcutis. This process is stimulated by thyrotropin receptor antibody-mediated cytokine release and activated Th1 cells [3]. Classical clinical manifestation includes peau d’orange appearance and non-pitting edema. These lesions are usually confined to the pretibial area but can occur at any other sites. The differential diagnosis includes erythema nodosum, keloid, and stasis dermatitis. Nodular variant of pretibial myxedema is generally considered self-limited. However, our case presents the variable appearance of post-radioactive iodine treatment dermopathy that was partially resistant to multimodal treatment approach.
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com/
For more details JOJ Dermatology & Cosmetics (JOJDC) please click on: https://juniperpublishers.com/jojdc/index.php
For more about Juniper Publishers Please click on: https://juniperpublishersblog.wordpress.com/

Comments
Post a Comment