Surgical Site Infections: Risk Factors and Post-Discharge Burden - Mini Review
Juniper Publishers- JOJ Dermatology & Cosmetics
Abstract
Despite decades of attention and advances in medical treatments, surgical site infections (SSI) remain a significant problem to patients. Surprisingly, the reported incidence of SSI has not changed appreciably in the past five decades. If not handled properly, these wounds may have a very poor prognosis and cause serious physical and psychological harm to patients, which adds to morbidity to patient during the course of treatment, In this review, we aim to identify the risk factors for SSIs and post discharge readmission morbidity to the patient
Keywords: Surgical Site Infections psychological harm Morbidity Control and Prevention American Society of Anaesthesiologists
Introduction
Surgical site infections (SSIs) are associated with increased morbidity and mortality. Although the quality of medical and surgical care has improved remarkably, the incidence of SSIs has not been decreasing in recent years. If not handled properly, these wounds may have a very poor prognosis and cause serious physical, economical and psychological harm to patients. SSI are more likely to have an extended hospital stay with additional economic costs, mainly attributable to the extended length of stay. Indirect costs, such as loss of productivity by the patient and an increased burden on their careers, further add to the economic cost of SSI to healthcare systems, which adds to morbidity to patient during treatment [1]. While the global estimates of surgical site infection (SSI) have varied from 0.5%-15%, studies in India have consistently shown higher rates ranging from 23%-38%. Among all surgical procedures, several risk factors of SSI have been identified, including length of surgery >180 minutes, wound classification according to the Centers for Disease Control and Prevention (CDC) guideline higher than class III, and an American Society of Anesthesiologists (ASA) score >3 [2]. In this review, we aim to identify the risk factors for SSIs and post discharge readmission morbidity to the patient.
Definition
The definition given as per CDC guidelines describes three levels of SSI [3]
a) Superficial incisional, affecting the skin and subcutaneous tissue. These infections may be indicated by localised signs such as redness, pain, heat or swelling at the site of the incision or by the drainage of pus.
b) Deep incisional, affecting the fascial and muscle layers. These infections may be indicated by the presence of pus or an abscess, fever with tenderness of the wound, or a separation of the edges of the incision exposing the deeper tissues.
c) Organ or space infection, which involves any part of the anatomy other than the incision that is opened or manipulated during the surgical procedure, for example joint or peritoneum. These infections may be indicated by the drainage of pus or the formation of an abscess detected by histopathological or radiological examination or during re-operation
Risk factors
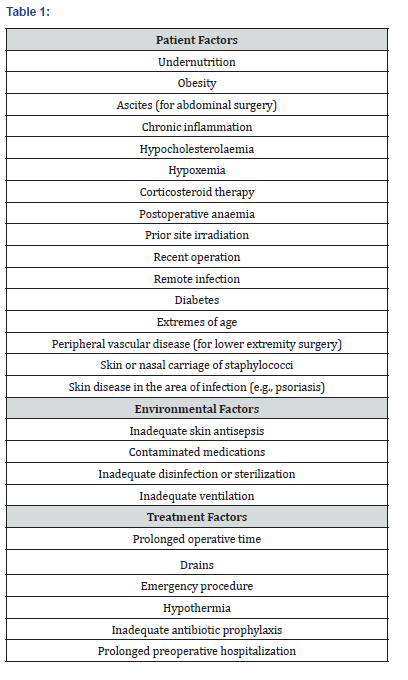
Numerous factors determine whether a patient will develop an SSI, including those related to the patient, environment, and treatment as shown in Table 1.
SSI and Hospital Re-Admission
One factor that has had significant impact on SSI diagnosis is the overall reduction in hospital stay. A population-based retrospective cohort study done by Daneman et al. [4] including more than 600,000 surgical cases from multiple specialties, reported an overall 30-day SSI rate of 13.5% confirms its high implication in patients. Interestingly, more than half of SSIs (58%) were diagnosed after hospital discharge. The study also suggested that post-discharge SSIs were associated with increased re-operation rates, emergency department visits, hospital re-admissions, and death. Previously validated risk indices for health-care–associated infection (HAI), however, based on patient characteristics and procedure length, failed to accuratelypredict patients at risk for the development of post-discharge SSI [5]. Similar results were found in a prospective cohort study of 1,506 general surgery patients in Spain. This single center study, conducted at a tertiary center, showed an overall SSI rate of 14.8%. The authors compared patients with a diagnosis of SSI during the index hospitalization (7.7%) with those with an SSI diagnosis after discharge (7.1%). While their identification of risk factors for development of in hospital SSI was consistent with known models (American Society of Anesthesiologists [ASA] physical status classification, severity of illness, National Health Safety Network of the Center for Disease Control [CDC], and Study on the Effectiveness of Nosocomial Infection Control [SENIC] index .Patients in whom post-discharge SSI developed were, again, more comparable to those who never had SSI than to those in whom SSI developed before discharge. Body mass index was a significant factor for all SSI, but notably, a surgeon’s SSI rate was most strongly associated with development of in-hospital SSI, not post discharge SSI [5]. In the retrospective analysis of a single center’s NSQIP database done by Gibson et al. [6] in a total of 3,663 patients undergoing inpatient general surgical procedures, SSI developed in 9.9%; 48% of these patients received an SSI diagnosis after hospital discharge and 54% of this patient subset required re-admission found that delayed superficial and deep incisional SSIs were most likely to be discovered in the first week after discharge. This is consistent with previous studies and, given the paucity of proven risk models for delayed SSIs, offers a potential avenue for improvement in clinical outcomes [6]. For all patients developing SSI post discharge from hospital, there is always a potential high costs and morbidity suffered because of SSI. performed a systematic review of the current literature on SSI health-related quality of life and found no consistent methodology employed for collecting this type of data. All studies reviewed were consistent in the message that SSI posed a significant burden to patients, but there was no reliable SSI disutility estimate, and the heterogeneous burden of SSI contributes greatly to this problem [7]. In a retrospective matched outcomes study, Kaye et al. [8] examined the impact of SSI on patients age 65 and older. Of elderly patients with SSI, 8.6% died of the complication within 90 days, representing an odds ratio of 3.51. This is higher than the twofold estimate of death from SSI for non-elderly adults. Poor pre-operative functional status and age over 80 years were significant predictors of death in this study. In addition, there was an average increase hospital stay of greater than 14 days [8]. In most types of surgical procedures, surgical site infections rates are higher in India those reported by the CDC in other countries. The Economic burden of Readmission or prolonged stay on patient is associated with high financial morbidity. To prevent all this Post discharge burden there are various guidelines, protocols and risk stratification, but is beyond the scope of this article.
Conclusion
While the global estimates of SSIs have varied from 0.5% to 15%, studies in India have consistently shown higher ratesranging from 23%-38%. SSIs are common complications which follow all types of operative procedures. If not handled properly, these wounds may have a very poor prognosis and cause serious physical, economical and psychological harm to patients. There are various risk factors which can lead to SSI and there are various guidelines, protocols and risk stratification to prevent it. So, prevention of SSI is an important aspect of health care sector.
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com/
For more details JOJ Dermatology & Cosmetics (JOJDC) please click on: https://juniperpublishers.com/jojdc/index.php
For more about Juniper Publishers Please click on: https://juniperpublishersblog.wordpress.com/

Comments
Post a Comment