Purpura Fulminanis- Juniper Publishers
Juniper Publishers- JOJ Dermatology & Cosmetics
Abstract
Purpura Fulminanis (PF) is an emergency progressive
thrombotic disorder in which there is skin necrosis, Disseminated
Dntravascular Coagulation (DIC) and multiorgan failure. It may
complicate severe sepsis or may occur as an autoimmune response to other
infection as varicella. Also, it may associate with severe heritable
deficiency of protein C or protein S. PF is a rapidly fatal disease, so
it needs rapid diagnosis and management promptly. We present a case of
purpura fulminanis who died, unfortunately, after 8 days due to severe
sepsis.
Keywords:
Purpura Fulminanis; Disseminated Dntravascular Coagulation; Coronary
Artery Bypass Grafting; Disseminated Intravascular Coagulation;
Intensive Care Unit; Laboratory Investigations; Neutrophilic
predominance; creatinine; Histological Findings; Methylprednisolone;
Immunoglobulin; Warfarin-Induced Skin Necrosis; Warfarin-induced skin;
pathophysiology; Thrombotic Thrombocytopenic purpura
Abbrevations:
PF: Purpura Fulminanis; DIC: Disseminated Dntravascular Coagulation;
CABG: Coronary Artery Bypass Grafting; DIC: Disseminated Intravascular
Coagulation; ICU: Intensive Care Unit; PTT: Partial thromboplastin time;
WBC: White blood cell count
Case Report
Male patient, 73years old, presented to the Emergency
Department with coffee ground vomiting (5 times) associated with
abdominal pain and melena. He was diabetic, hypertensive, and had
chronic obstructive pulmonary disease and had past history
of Coronary Artery Bypass Grafting (CABG). After three days, he
developed septic shock which was associated with coma, purpuric rash and
overt Disseminated Intravascular Coagulation (DIC), and renal
impairment. He was managed by fluid resuscitation and intubation and was
transmitted to Intensive Care Unit (ICU).
On Examination
He was afebrile, his temperature was 36.8°C, his blood
pressure was 104/68mmHg with a heart rate of 71 beats/minute,
respiratory rate of 17 breaths/minute, and oxygen saturation of
94% in room temperature air. He had generalized deep purpuric
lesions on both hands, upper and lower extremities, some of
lesions were blackish purpuric in color with tense blisters as in
dorsum surfaces of both hands, as shown in Figure 1 & 2.


Laboratory Investigations
As regard his complete blood count
The clinically significant results are as follows:
White blood cell count (WBC) of 6.97k/μL (N) (n4 – 10k/
μL), with a neutrophilic predominance of 93.3% (n40-80%), Red
blood cell count (RBC) of 4.02M/μL (L) (n4.5-505M/μL) with a
hemoglobin of 9.9gm/dl (L), hematocrit of 32.90% (L) (n40-50%),
Platelet count of 269 K /μL (N) (n150-410 K/μL).
As regard his chemistry
His random glucose of 322mg/dL (high) (n70-140mg/dL),
blood urea of 154.60mg/dL (high critical) (n 8.6-10.20mg/dL),
creatinine of 2.99mg/dL (high) (n 8.6-10.20mg/dL), normal
SGOT (AST) (22μ/L) (n 0-35μ/L), normal SGPT (ALT) (14μ/L) (n
0-41μ/L), normal bilirubin (total) (0.476mg/dL) (n 0-1.1mg/dL),
low total protein (5.93g/dL) (n 6.6-8.7g/dL) and low albumin of
3.67g/dL (L) (n3.97-4.94g/dL), low chloride (92.20mmol/L) (n98-
107mmol/L), low sodium (132mmol/L) (n135-151mmol/L), and
High critical potassium (8.02mmol/L) (n3.4-5.1mmol/L).
As regard coagulation profile
Partial thromboplastin time (PTT) was (84.40 sec.) (high)
(n26-40 seconds), ThromboPlastin time (PT) of (16.60 sec.) (high)
(n11-14.5 seconds), and INR of 1.30% (high) (n0.8-1.2%).
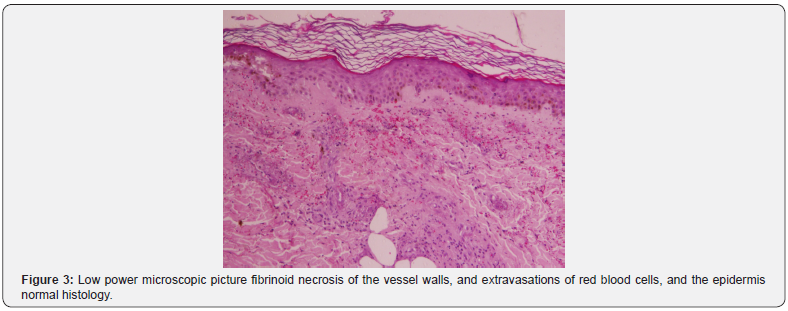
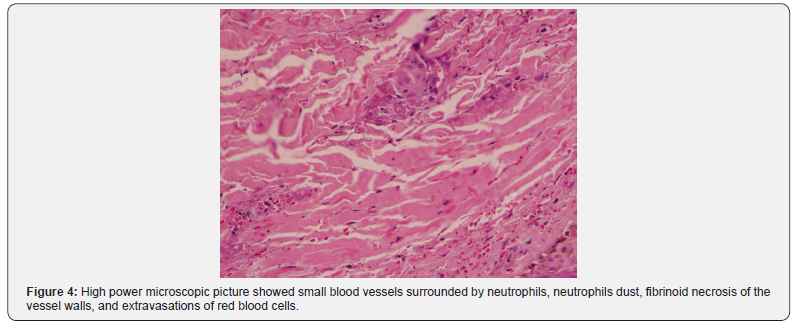
Histological Findings
Sections examined from skin biopsy showed dermis with
small blood vessels surrounded by neutrophils, neutrophils dust,
fibrinoid necrosis of the vessel walls, and extravasations of red
blood cells. The overlying epidermis showed normal histology, as
shown in Figure 3 & 4.
Discussion
The patient was admitted at the ICU, and his high blood
sugar was controlled by insulin, his purpura was treated by the
rheumatologist with methylpredisolone 750mg i.v. daily for three
days, and was treated by heparin and broad-spectrum antibiotics,
but unfortunately, he died due to severe sepsis after 8 days.
Although, the histopathological examination suggested diagnosis
of leuckcytoclastic vasculitis, the case was presented clinically as
a purpura fulminans, and the methylpredisolone 750mg i.v. daily
for three days which was prescribed by the rheumatologist was
wrong because it flared the sepsis, and the best medication was
fresh plasma and immunoglobulin G.
Differential diagnosis
Purpura fulminans
Purpura Fulminans (PF) is a life-threatening disorder of
acute onset characterized by cutaneous haemorrhage and
necrosis caused by disseminated intravascular coagulation and
dermal vascular thrombosis. Three distinct categories can be
identified: inherited or acquired abnormalities of protein C or
other coagulation systems, acute infectious PF, and idiopathic
[1]. Its cardinal manifestations are presence of circumscribed
ecchymosis of skin and symmetrical gangrene of the extremities
with coagulation abnormalities suggestive of disseminated
intravascular coagulation [2]. Late findings in necrotic areas are
the formation of vesicles and bullae, which mark the development
of haemorrhagic necrosis, and finally firm eschar, which ultimately
sloughs. The distal extremities are often most severely involved,
usually in a symmetric manner, probably due to fewer collateral
channels for tissue perfusion, and the relatively greater impact of
circulatory collapse on perfusion of distal vascular beds [3].
Development of systemic consumptive coagulopathy is a defining
feature of PF, which distinguishes it from other forms of
skin necrosis due to dermal vascular occlusion such as warfarin
or heparin induced skin necrosis, thrombotic thrombocytopenic
purpura, cryoglobulinaemia, antiphospholipid syndrome, or
paroxysmal nocturnal haemoglobinuria. Fibrinogen, coagulation
factors (factor V and VIII), and platelets are consumed in ongoing
thrombosis and fibrinolysis. Prothrombin time, partial thromboplastin
time are prolonged; fibrin degradation products are elevated,
and protein C, protein S and antithrombin III are reduced. The
histopathological hallmarks of PF are dermal vascular thrombosis
and secondary haemorrhagic necrosis [4], which are identical
to Schwartzman reaction [5]. Vasculitis, including a perivascular
neutrophilic infiltrate, is a characteristic feature of acute infectious
PF, which distinguishes it from other forms of PF.
Leuckcytoclastic vasculitis
Leukocytoclastic vasculitis (LCV), also called hypersensitivity
vasculitis, is a small-vessel vasculitis its incidence rate is about
30 cases per million people per year and affect men and women
in equal numbers [6,7]. The skin is the organ most commonly
involved by LCV and its presentation is a painful, burning rash
predominantly in the lower extremities, with up to one-third of
patients presenting with trunk and upper extremity involvement.
[3] The most common skin manifestation of LCV is palpable
purpura [8]. Other skin manifestations include maculopapular
rash, bullae, papules, plaques, nodules, ulcers, and livedo
reticularis. Patients with LCV may also present with arthralgias or
arthritis involving the knees or ankles [9].
Meningococcemia
The clinical pattern of meningococcemia varies. Persons with
meningococcal disease may present with a nonspecific prodrome
of cough, headache, and sore throat. After a few days of upper
respiratory symptoms, the temperature rises abruptly, often after a
chill. malaise, weakness, myalgia, headache, nausea, vomiting, and
arthralgia are common presenting symptoms. A skin rash, which
is essential for recognizing meningococcemia, is the characteristic
manifestation. The skin rash may advance from a few ill-defined
lesions to a widespread petechial eruption within a few hours.
Meningococcemia’s potential rapidity of progression cannot be
stressed enough. In fulminant meningococcemia, a hemorrhagic
eruption, hypotension, and cardiac depression, as well as rapid enlargement of petechiae and purpuric lesions, may be apparent
within hours of the initial presentation [10].
Warfarin-Induced Skin Necrosis
Warfarin inhibits the activation of vitamin K–dependent
clotting factors II, VII, IX, and X and the anticoagulant proteins C
and S [11-13]. Warfarin-induced skin necrosis is a rare (0.01%-
0.1%) but serious complication that usually occurs within the first
several days following warfarin initiation, although case reports
have described this phenomenon later in therapy as well [12-15].
This adverse drug reaction appears to be associated with larger
doses of warfarin [13]. The pathophysiology is not well understood;
however, it is theorized that this complication is due to the initial
procoagulant state that warfarin causes, leading to the formation
of fibrin clots within the microvasculature. These blood clots cause
interruption in blood supply to the skin, resulting in necrosis.
The general progression of warfarin-induced skin necrosis is as
follows: pain and erythema; petechial hemorrhages; red, purple,
blue, or black discoloration; necrosis; and hemorrhagic blisters
and/or bullae. Early recognition of symptoms and treatment are
vital to preventing substantial morbidity associated with warfarininduced
skin necrosis; however, due to its rare occurrence,
appropriate treatment has not been well established [12].
Thrombotic thrombocytopenic purpura
Thrombotic thrombocytopenic purpura (TTP) is a rare
blood disorder characterized by clotting in small blood vessels
(thromboses), resulting in a low platelet count [16]. In its fullblown
form, the disease consists of microangiopathic hemolytic
anemia, thrombocytopenic purpura, neurologic abnormalities,
fever and Renal disease [17].
TTP can affect any organ system, but involvement of the
peripheral blood, the central nervous system, and the kidneys
causes the clinical manifestations. Patients with TTP typically
report an acute or subacute onset of symptoms related to
neurologic dysfunction, anemia, or thrombocytopenia. The
neurologic manifestations include alteration in mental status,
seizures, hemiplegia, paresthesias, visual disturbance, and
aphasia. Fatigue may accompany the anemia. Severe bleeding from
thrombocytopenia is unusual, although petechiae are common
[18,19].
Conclusion
Purpura fulminanis manifestations are confusing with many
diseases, so we should differentiate it promptly from other
diseases to avoid misdiagnosis, delay management, mistreatment,
and sudden death as occurred in our presented case.
For more Open Access Journals in Juniper Publishers please click on:
For more details JOJ Dermatology & Cosmetics (JOJDC) please click on: https://juniperpublishers.com/jojdc/classification.php

Comments
Post a Comment