Bulbous and Globose-Merkel Cell Carcinoma
Editorial
Merkel cell carcinoma is an infrequently discerned, aggressive, primary cutaneous carcinoma of neuroendocrine origin. Additionally designated as trabecular carcinoma and initially scripted by Toker in 1972, tumefaction simulates numerous benign and malignant cutaneous lesions. Localized disease is common, followed by regional lymph node or distant metastasis. Spontaneous regression of disease is exceptional. Disease-associated mortality is significant [1,2].
Primary cutaneous Merkel cell carcinoma can be segregated from metastatic cutaneous neuroendocrine carcinoma with pertinent clinical and histological examination along with immunohistochemistry. Majority of neoplasms may be engendered due to infection with Merkel cell polyomavirus. Few instances emerge due to ultraviolet radiation induced activation of diverse onco-genetic pathways [1,2]. Generally, elderly Caucasian population >70 years and immunosuppressed individuals are incriminated. A male predominance is observed [1,2].
Factors contributing to emergence of Merkel cell carcinoma are advanced age, chronic, persistent exposure to sunlight or ultraviolet radiation, fair skin and immunosuppression as encountered with organ transplantation, HIV infection, chronic lymphocytic leukaemia or autoimmune disorders [1,2].
Merkel cell carcinoma exemplifies varying genetic profiles for neoplasms which are immune reactive to MCPyV+ and immune non-reactive to MCPyV- [1,2].
Tumefaction immune non-reactive to MCPyV-demonstrates genetic mutations of TP53 and RB1, ultraviolet signature mutations and elevated tumour mutation burden [1,2]. Merkel cell carcinoma occurs within cutaneous surfaces exposed to sunlight such as head and neck, extremities, or trunk [1,2].
Generally, clinical appearance is non-specific. Tumefaction may manifest as a painless, briskly expanding, flesh-coloured or reddish-violaceous, cutaneous nodule. Characteristic clinical features as a rapidly progressive, asymptomatic nodule devoid of tenderness may emerge.
Merkel cell carcinoma can be appropriately staged with assessment of tumour magnitude, depth of tumour invasion, incrimination of localized or regional lymph nodes and disseminated metastasis [1,2]. Factors associated with inferior prognostic outcomes are advanced disease at initial representation, incrimination of male subjects > 60 years, disease occurrence within head and neck, immunosuppression, and neoplasms non-reactive to Merkel cell polyomavirus [1,2].
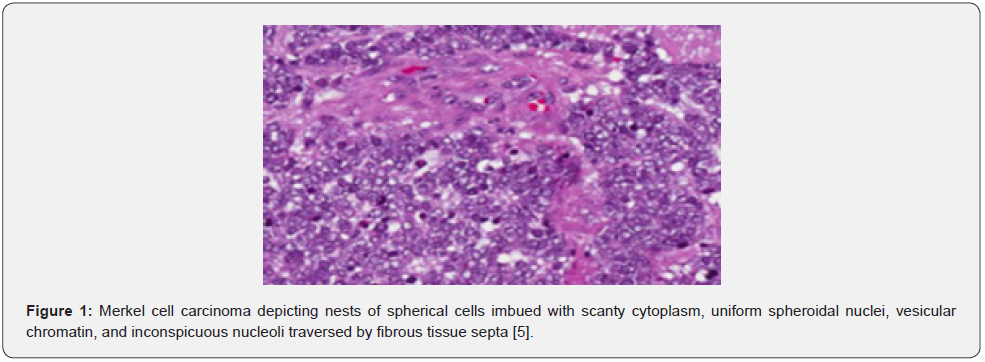
Cytological specimens are hyper-cellular and constituted of singularly dispersed or disorganized, cohesive aggregates of miniature to medium-sized neoplastic cells with nuclear moulding. Neoplastic cells are imbued with uniform, spherical or elliptical nuclei with fine, stippled chromatin, inconspicuous nucleoli, scanty cytoplasm, and enhanced nucleo-cytoplasmic ratio. Apoptotic bodies and mitotic figures are frequent. Focal necrotic debris may be discerned [1,2].
Grossly, a fleshy, tan, or brown, variably ulcerated, nodular lesion with poorly defined perimeter is observed [1,2]. Upon microscopy, an expansible, nodular tumefaction or diffusely infiltrating dermal neoplasm appears to variably expand within subcutaneous tissue. Neoplasm is configured of an admixture of tumour cell nodules, sheets, nests, or trabeculae. An intra-epidermal neoplastic component may be occasionally discerned [1,2].
Miniature, spherical, bluish tumour cells imbued with scanty cytoplasm, spherical to elliptical nuclei with finely dispersed, ‘salt-and-pepper’ chromatin, inconspicuous nuclei and an enhanced nucleo-cytoplasmic ratio constitute the neoplasm. Mitotic figures and apoptotic bodies are prominent. Nuclear moulding is variable and crush artefacts may ensue. Majority of neoplasms exhibit a singular neuroendocrine morphology and are designated as ‘pure’ Merkel cell carcinoma [1,2] (Figure 1 -2).

Few tumours emerge as combined Merkel cell carcinoma with neuroendocrine features amalgamated with focal divergent differentiation as squamous cell or sarcomatoid carcinomas [1,2].
Merkel cell carcinoma may be associated with various cutaneous neoplasms, commonly with in situ or invasive squamous cell carcinoma [1,2] (Table 1).

In transit metastasis is comprised of intra-lymphatic tumour deposits discontinuous from primary lesion and is situated between primary lesion and draining regional lymph nodes or distal to primary lesion.
Ultrastructural examination exhibits intracytoplasmic, membrane bound, dense core neurosecretory granules along with para-nuclear aggregates of keratin filaments [3,4]. Merkel cell carcinoma is immune reactive to pan-cytokeratin, CAM5.2, AE1/ AE3, CK20, chromogranin, synaptophysin, CD56, CD99, neuronspecific enolase, neuro-filament, MCPyV, PAX5, TdT, bcl2 or FLI1. Merkel cell carcinoma is immune non-reactive to CK7, TTF1, CDX2, S100 protein, CD45 or vimentin [3,4].
Merkel cell carcinoma requires segregation from neoplasms such as basal cell carcinoma, metastatic neuroendocrine carcinoma, lymphoma, leukaemia, small cell variant of malignant melanoma, Ewing’s sarcoma, cutaneous squamous cell carcinoma, dermatofibroma, keratoacanthoma or various dermatological manifestations of metastatic carcinomas [3,4].
Upon computerized tomography(CT), iso-attenuating or hyper-attenuating soft tissue foci are observed [3,4]. Magnetic resonance imaging (MRI) depicts image enhancement with contrast administration [3,4]. Positron emission computerized tomography (PET-CT) with fluoro-deoxyglucose displays avid, hypermetabolic activity [3,4]. A multidisciplinary approach is recommended for optimal therapy [3,4]. Surgical excision or tissue sampling with cogent microscopic evaluation is diagnostic and curative [3,4].
Localized surgical excision with removal of broad perimeter of uninvolved tissue can be suitably adopted [3,4]. Inoperable tumefaction may benefit with single modality radiotherapy. Sentinel lymph node biopsy is optimal for evaluating and treating neoplasms devoid of regional lymph node metastasis. Adjuvant radiotherapy may or may not be employed [3,4].
Immune checkpoint blockade therapy with targeting of PDL1 / PD1 pathway is beneficial for treating neoplasms of advanced stage [3,4]. Adjuvant chemotherapy is usually ineffective. Palliation may be achieved with chemotherapy [3,4]. Exclusion of preceding cutaneous malignancy and possible distant metastasis of non-cutaneous primary tumours is necessitated [5,6].
References
- Fennig S, Landman Y, Brenner R, Billan S, Fenig E (2022) Merkel cell carcinoma in lymph nodes with and without primary origin. Cancer Med (6): 1484-1489.
- Mesa F, Cardona M, Mesa C, Restrepo R, Andrés Echeverri J (2022) Merkel cell carcinoma in the hand. Report of two cases. Case Reports Plast Surg Hand Surg 9(1): 41-45.
- Villani A, Fabbrocini G, Costa C, Annunziata MC, Scalvenzi M (2019) Merkel Cell Carcinoma: Therapeutic Update and Emerging Therapies. Dermatol Ther (Heidelb) 9(2): 209-222.
- Brady M, Spiker AM (2022) Merkel Cell Carcinoma of the Skin. Stat Pearls International Treasure Island, Florida.
- Image 1 Courtesy: Research gate.
- Image 2 Courtesy: Hindawi.com.
To Know More About JOJ Dermatology & Cosmetics Please click on:
https://juniperpublishers.com/jojdc/index.php
For more Open Access Journals in Juniper Publishers please click on:
https://juniperpublishers.com/index.php


Comments
Post a Comment