Single Plaque-Type Chromoblastomycosis: Great and Sustained Response with Itraconazole Plus Cryosurgery
Juniper Publishers- JOJ Dermatology & Cosmetics
Abstract
We present a 72-years-old male patient, resident in a urban area, with a chronic cutaneous ulcer on the left forearm, diagnosed with chromoblastomycosis, treated with a combination therapy of oral itraconazole and cryocirurgery, with 6-months follow up after treatment.
Keywords:Black Fungi; Chromoblastomycosis; Chromomycosis; Melanized Fungi; Muriform (Sclerotic) Cells
Introduction
The Chromoblastomycosis (CBM) is a chronic fungal infection caused by the traumatic implantation of demeaceous fungi of the Herpotrichiellaceae family on the skin and subcutaneous cellular tissue [1-3]. These fungi are more common in tropical and subtropical areas, and can be found in the soil, in vegetation and decomposing wood [1,2]. It is more common in male rural workers, lumbermen or sellers of agricultural products [4]. Brazil is the second country in number of cases, being found throughout its entire territory [2,5].
History and Clinical Manifestations
Male pacient, 72 years, urban dweller, retired (former bricklayer), sought medical attention due to injury to the left forearm. It started 6 months earlier as a papulo-pustular lesion, wich progressed slowly and progressively to an erythematous plaque, with a rough surface; asymptomatic. Upon examination, an infiltrated, erythetous-keratotic plaque was indentified, with well-defined edges and an irregular, slightly verrucous surface, measuring about 5.0cm in the largest diameter (Figure 1). Dermoscopy indentified black dots (Figure 2). When questioned, he associated the injury with a sharp puncture trauma during the repair of the house fence. With the hypothesis of subcutaneous mycosis (chromomycosis and sporotrichosis), tuberculosis, in addition to neoplasia (squamous cell carcinoma), an incisional biopsy was performed.
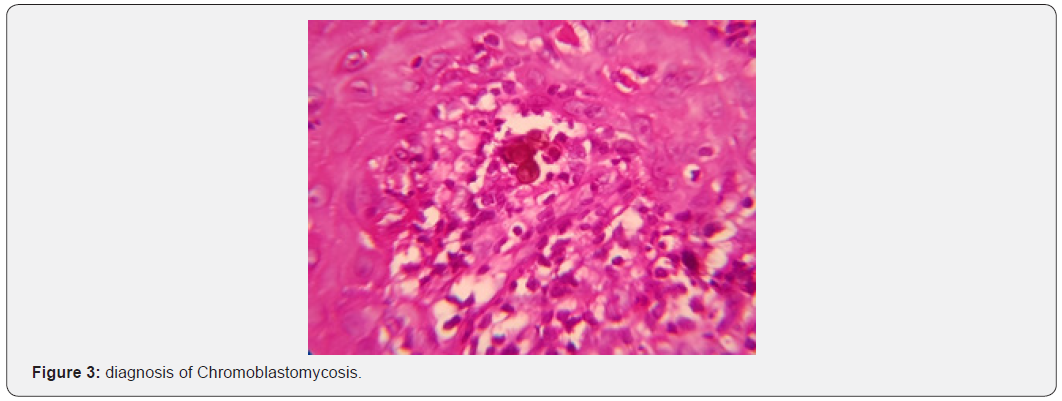
Histopathological examination showed chronic granulomatous dermatitis associated with pseudoepitheliomatous hyperplasia of the epidermis. In the dermis, the presence of sclerotic cells (Figure 3), confirming the diagnosis of Chromoblastomycosis. Fungal culture isolated the demeaceous fungus Fonsecaea Pedrosoi. Treatment with Itraconazole 200mg/day for 6 months, associated with 4 sessions of Cryosurgery (local infiltrative anesthesia, tip B, intermittent jets, 2 cycles, thawing time 2 times that of freezing) at 1-month intervals. Apparent clinical cure 6 months after the end of treatment (Figure 4).

Discussion
CBM begins with a primary lesion at the traumatic fungus inoculation site, usually oligosymptomatic, delaying the demand for care [2,4]. A papule is noted, usually in areas of exposed skin, wich grows in a centrifugal manner. There may be progression of the condition due to contiguity, in addition to lymphatic and/ or hematogenic dissemination [1,2,6]. It is classified clinically in 5 types: nodular, verrucous or verruciform, plaque, tumor and scar or atrophic. Possible complications are secondary bacterial infection, elephantiasis and carcinomatous degeneration [2,6]. The differential diagnosis is made with paracoccidioidomycosis, sporotrichosis, lacaziosis, leishmaniasis, mycetomas, leprosy, tuberculosis, atypical mycobacteriosis, prototecosis, in addition to squamous cell carcinoma [2].
Epidemiology assists in diagnosis, especially in endemic areas.4 This can be confirmed by visualization of the fungus in direct examination, in tissues with histopathological examination, in addition to culture isolation.5 The sclerotic (muriform) cells are pathognomonic for CBM, regardless of the causative species [2]. The treatment is difficult, with recurrence and chronic lesions being common.6 There is no gold standard of treatment. Some options are cryosurgery, carbon, dioxide laser, itraconazole, flucytosine, terbinafine, amphotericin B, fluconazole, posaconazole, imiquimod, super-satured potassium iodide and thermotherapy, used alone or in combination. The choice depends on the age and comorbidities of the pacient, as well as the location of the lesions [5]. Cryosurgery with liquid nitrogen and thermotherapy are suitable options for isolated and limites lesions [2]. Already the antifungals that have shown greater effectiveness are itraconazole and terbinafine for 6 to 12 months, preferably in higher doses, if tolerated [2].
Conclusion
We present an illustrative case of CBM, plaque shape, in an elderly man from an urban area, with a report after questioning trauma involving a wooden and wire fence, seeking to draw attention to this entity in the day-to-day of the dermatologist even if outside endemic area and without typical epidemiology. In parallel, a good therapeutic result is demonstrated with the association of surgical and medication techniques, which are accessible and well tolerated.
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com/
For more details JOJ Dermatology & Cosmetics (JOJDC) please click on: https://juniperpublishers.com/jojdc/index.php
For more about Juniper Publishers Please click on: https://juniperpublishersblog.wordpress.com/

Comments
Post a Comment