Palmoplantar Pustulosis with Subungual Pustules Treated with Arotinoid Ethyl Ester
Juniper Publishers- JOJ Dermatology & Cosmetics
Abstract
A 43-year-old Chinese man developed crops of pustules on soles for 7 months and subungual pustules for 6 months. Biopsy on the sole lesion revealed intraepidermal unilocular pustules filled with bulk of neutrophils. This case proved to be palmoplantar pustulosis with nail involvement. After 28-week treatment with arotinoid ethyl ester, all plantar and subungual lesions cleared completely. The treatment of PPP is challenge; especially for the subungual pustules are rare and difficult to be diagnosed and treated. Herein we report the case and effective therapy with literature review.
Keywords: Arotinoid ethyl ester Palmoplantar pustulosis Subungual pustules
Introduction
Palmoplantar pustulosis (PPP), synonymously as localized pustular psoriasis, is characterized by recurrent sterile pustules bilaterally and symmetrically on palms and soles. Nail changes in PPP are rare and difficult to be diagnosed and treated [1-4]. Arotinoid ethyl ester(p-[(E)-2-(5, 6, 7, 8-tetrahydro-5, 5, 8, 8-tetramethyl-2-naphthyl) propenyl]-benzoic acid ethyl ester), a member of polyaromatic retinoids, has shown the potent anti-psoriatic and anti-inflammatory effects at very low dosage level [5]. Here, we report a case of PPP with greenish subungual pustules, which were successfully treated with arotinoid ethyl ester.
Case Report
A 43-year-old Chinese man presented to our outpatient clinic with crops of pustules on soles for 7 months and pustules under fingernail plates for 6 months. Palms were spared. The patient had no complaint of pain or pruritus. The deformed nail plates with onycholysis developed for two months period. No systemic medication was given before. Physical examination showed multiple yellow to dark brown pustules and erythema on the bilateral soles (Figure 1). Under 3rd, 4th and 5th fingernails of right hand there were greenish subungual pustules from 1mm×3mm-3mm×8mm in diameter.
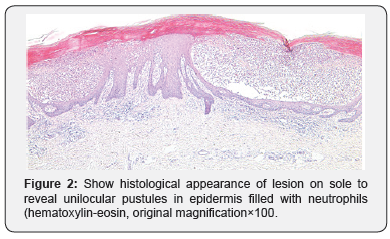
He was afebrile, his temperature was 36.8°C, his blood pressure was 104/68mmHg with a heart rate of 71 beats/minute, respiratory rate of 17 breaths/minute, and oxygen saturation of 94% in room temperature air. He had generalized deep purpuric lesions on both hands, upper and lower extremities, some of lesions were blackish purpuric in color with tense blisters as in dorsum surfaces of both hands, as shown in Figure 1 & 2. A diagnosis of PPP was made. The patient received arotinoid ethyl ester 0.03mg once daily. Plantar lesions and subungual pustules substantially improved in 3 weeks (Figure 3). No obvious side effects were observed except transient elevation of serum low density lipoprotein level and mild xerosis. After 28-week treatment, all lesions cleared completely. No relapse occurred at 1-year follow up visit (Figure 4 & 5).
Discussion
It was reported that subungual pustules were found in 20% patients with PPP, [2] and caused functional and physical restriction to the hand [3,6]. We reviewed our outpatients with PPP of a university hospital from 2000-2006. Among 178 subjects, one case with subungual pustules was identified. The incidence of PPP concurrent with subungual pustules was much lower than that reported before [2]. Perhaps the occurrence of subungual pustules was related to the regional and ethnic variation.
Pseudomonas aeruginosa infection and onychomycosis are important causes of chromonychia [7]. In our case, repeated Gram staining and cultures of subungual pus were negative for both fungi and pseudomonas aeruginosa.
Nail changes in PPP is resistant to treatment just like that in psoriasis [8]. Because of minimal drug absorption by nail plate, class I topical corticosteroids are usually ineffective even under occlusion [9,10] although Clobetasol in nail lacquer was reported effective for nail psoriasis [11]. Treatment alternately with calcipotriol and clobetasol propionate exhibited 77% mean improvement in nail changes of psoriasis [12]. Effective monotherapy with calcipotriol ointment (50mg/g) was observed in other study [13]. Rigopoulos et al. [14] treated nail psoriasis with 0.1% tazarotene cream under occlusion and observed a significant improvement. In addition, 5-fluorouracil ointment was used sporadically for nail psoriasis [15].
Acitretin, 10-25mg daily, in combination with PUVA, was effective in treatment of PPP with significant nail involvement [9]. Patients with nail psoriasis treated by cyclosporine, at 5-2.5mg/kg/d, exhibited a marked improvement in nail changes [16]. Arotinoid ethyl ester is a member of the third generation of retinoids. It exhibited potent therapeutic efficacy to induce differentiation, inhibit proliferation and suppress inflammation and keratinization. The therapeutic efficacy has been demonstrated in Darier’s disease, cutaneous T-cell lymphoma, psoriasis vulgaris and another dermatosis [17-20]. Side effects of arotinoid ethyl ester such as elevated triglyceride and low-density lipoprotein, mucocutaneous xerosis and skin exfoliation were reported; those were milder and less frequent than acitretin. As teratogenicity of arotinoid ethyl ester has been demonstrated in animal study, it should not be prescribed for pregnant women or child-bearing potential females [5].
In our patient, after 28-week treatment with arotinoid ethyl ester, all plantar and subungual lesions were cleared completely with mild side effects. We suggest that arotinoid ethyl ester is a promising candidate in the therapy of nail changes in PPP. Because of limited number of the patient, the efficacy and safety of arotinoid ethyl ester on nail involvement of PPP needs to be further validated in a large-scale study.
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com/
For more details JOJ Dermatology & Cosmetics (JOJDC) please click on: https://juniperpublishers.com/jojdc/index.php

Comments
Post a Comment