Pemphigus Vulgaris and Infections: A Retrospective Study on Hundred Patients Presenting as Inpatient Cases at Mayo Hospital Lahore
Juniper Publishers- JOJ Dermatology & Cosmetics
Abstract
Background: Autoimmune process and immunosuppressive therapy of pemphigus vulgaris would predispose the patients to infections
Aim: We aimed to study the prevalence of infection and pathogenic agents in pemphigus vulgaris patients admitted to dermatology service.
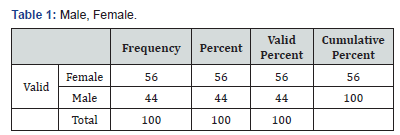
Material and methods: This retrospective study was conducted on 155 pemphigus vulgaris patients (68 males, 87 females) (Table 1) admitted to dermatology service between 2009 and 2011. In this study, the diagnosis of pemphigus vulgaris was confirmed by light microscopic and direct immunofluorescence findings. Data were collected through a questionnaire.
Results: Out of 155 pemphigus vulgaris patients, 33 had infection at admission and 9 acquired nosocomial infection. In addition, 37 cases of oral candidiasis and 15 cases of localized herpes simplex were recorded. Totally, 94 cases of infection were recorded. The occurrence of infection was significantly related to the severity of disease, number of hospital admissions, and presence of diabetes mellitus. The most common pathogenic germs isolated from cultures were Staphylococcus aureus and Escherichia coli.
Conclusion: Severity of pemphigus vulgaris and diabetes were directly related with tendency to infections. Staphylococcus aureus and Escherichia coli were the most common pathogenic agents. Due to limitations of retrospective study, a prospective study is recommended.
Keywords: Pamphigus Vulgaris Acantholysis Sepsis Cellulitis
Introduction
Pemphigus vulgaris (PV) is an organ-specific autoimmune bullous disease which is characterized by loss of cell adhesion (acantholysis) and blister formation [1,2]. This disease is proven to be an autoimmune phenomenon [1-3]. Considering this etiology, immunosuppressive drugs are the main treatments available for this disorder. Infections are important complications in these patients which are attributed to disruption of the epidermal barrier (a part of innate immunity) due to the disease itself and immunosuppression induced by treatment [4,5]. There are many reports regarding predisposition to infections due to immunosuppressive therapy and the immunocompromised state of pemphigus patients [6,7]. PV has a high prevalence in Pakistan; in this regard, we have studied this autoimmune disease from many different points of view [8-10]. The aim of the present study was to determine the rate of infection in PV patients admitted to dermatology inpatients service through a retrospective study held at mayo hospital indoor department of dermatology.
Material and Methods
This retrospective study was performed on 100 PV patients (56 females, 44 males) admitted to the dermatology department of Mayo Hospital of Lahore in Pakistan, between 2016 and 2018. The mean age of patients was 39 yrs. (range: 14-70) of 100 admitted PV patients in indoor department of mayo hospital Lahore
Patients with a clinical diagnosis of PV with compatible histopathology and direct immune fluorescence (DIF) findings confirming the clinical diagnosis of PV entered the study. Light microscopic and direct immunofluorescence findings in favor of pemphigus vulgaris were suprabasal bullae and acantholysis and IgG and C3 depositions in the intercellular regions of epidermis, respectively. The severity of PV was evaluated by a “severity index for pemphigus,” namely, mild, moderate, and severe [11]. All of the PV patients contributing to this study (mild, moderate, and severe) were hospitalized in the dermatology wards of Mayo Hospital regardless of severity of the disease. Accordingly, 4 patients (4%) had mild, 25 pts (25%) had moderate, and 48 patients (48%) had severe, and 23 patients (23%) very severe forms of the disease.
Regardless of the severity of pemphigus, the patients were treated with 2mg/kg/day prednisolone and 2.5mg/kg/day azathioprine [12]. In this study, 04 patients with mild disease with upper limit of the normal range of liver function tests (aspartate aminotransferase=2U/L, alanine transaminase=41U/L) or lower limit of the normal range of white blood cells count (4×103/ microliter or less) who were not suitable for azathioprine adjuvant therapy were treated with 2mg/kg/day prednisolone alone. 100 patients with mild, moderate, and severe disease (mild=04, moderate=25, and severe=71) were treated with 2mg/kg/day prednisolone and 2.5mg/kg/day azathioprine. 10 PV patients with moderate and severe disease (moderate = 10, severe=10) with upper limit of the normal range of liver function tests who were not suitable for azathioprine adjuvant therapy were treated with 2mg/kg/day prednisolone and 2g/day (4×500mg/day tablet) mycophenolate mofetil [13].The phenotype of PV recorded in order of frequency was mucocutaneous in 70 (70%), cutaneous in 19 (19%), and mucosal phenotype in 11 patients (11%).
Demographic data including age, gender, number of admissions, severity of the disease, underlying medical disorders such as history of diabetes and hypertension, treatment protocols, and infections recognized during the admission period were registered in the appropriate questionnaires.
Statistical Analysis
Data were collected by questionnaire and analyzed by statistical software, SPSS.
Results
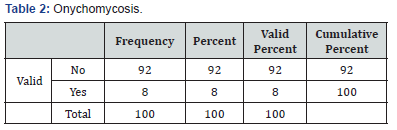
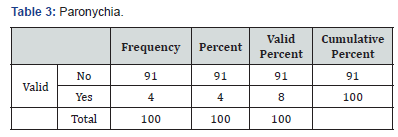
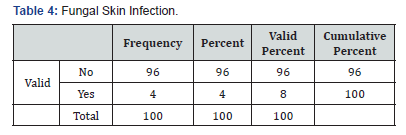
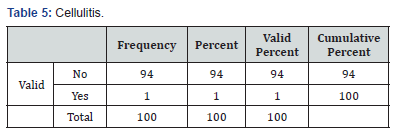
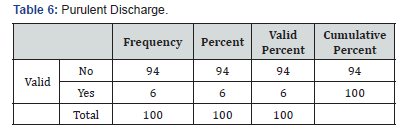
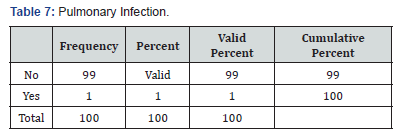
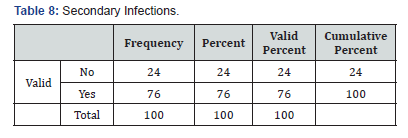
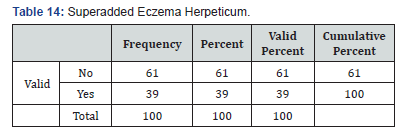
In total 100 cases of pemphigus vulgaris infections were recorded. Forty-eight patient had a clinical diagnosis of oral candidiasis and onychomycosis (Table 2) was seen in 8 patients’ eczema herpeticum was seen in 39 patents paronychia (Table 3)was seen in 9 patients, fungal skin infection (Table 4) was seen in 4 patients, cellulitis (Table 5) of abdominal wall was seen in 1 patient and 4 patients went into sepsis. Purulent discharge (Table 6) from erosion was seen in 24 patients and 1 patient died of sepsis, 2 patients were having pulmonary infection (Table 7).
Discussion
PV is a well-known autoimmune disease [14]. Nowadays, the relationship between autoimmunity, immunodeficiency, and infection is well recognized. It is believed that autoimmunity and immunodeficiency are not separate entities, but rather some connection exists between them [15,16]. On the other hand, hospitalization in addition to immunosuppressive therapy would predispose the PV patients to infection (Table 14).
Our search in the literature revealed some similar studies performed in other countries [6]. In our study, 76% of PV patients had infections, while in the study of Belgnaoui et al., 68% of patients had infections. Overall, our results are similar to the study of Belgnaoui et al. [6] The small differences between the two studies may be due to differences in severity of disease (Table 9,10) and duration of hospitalization [6].
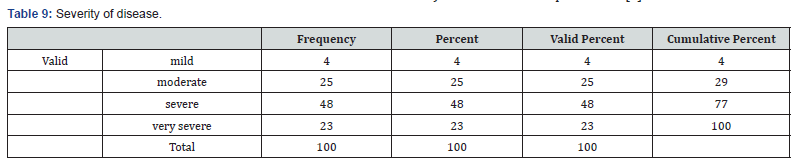
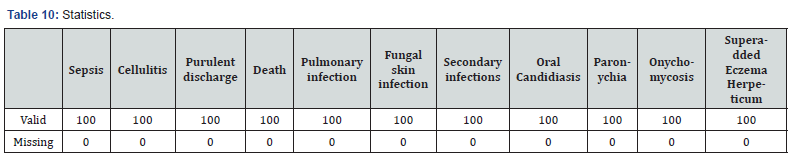
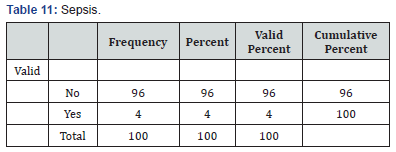
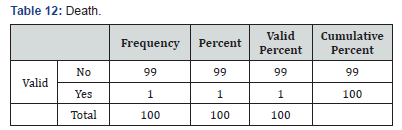
The study of Ljubojević et al. [17] on 159 PV patients during 19 years revealed several complications associated with high doses of corticosteroids and immunosuppressive therapy [17]. These complications were as follows: skin infection in 26 patients (16.35%), sepsis (Table 11) in 9 patients (5.66%), and 14 patients (8.81%) died during the period of hospitalization. With regard to skin infection, the results of the Ljubojević et al. [17] study are similar to those of the present study. The absence of sepsis and death (Table 12) in our study may be due to the small number of patients with severe PV and the shorter period of our study. In our study, the occurrence of infection had a direct relationship with disease severity, and the difference between mild and severe wassignificant. In Ljubojević et al. [17] study, severe cutaneous and mucosal involvement was also consistent with a higher mortality rate [17]. Mourellou et al. [18] followed 48 patients for 11 years; they concluded that complications and mortality rate of PV were related to the severity of PV. Our study is consistent with the study by Mourellou et al. [18]. In the current study, the rate of infection in PV patients with diabetes was significantly higher than in nondiabetics (P=0.044). Belgnaoui et al. [6] also reported more severe bacterial infection in diabetics PV patients [6].
In our study, the rate of infection in patients receiving immunosuppressive adjuvants plus systemic steroids was not significantly different from patients receiving corticosteroids alone. This means that all PV patients receiving corticosteroids (with or without adjuvant immunosuppressive) are prone to infections. It should be noted that we did not include the PV patients treated with rituximab (which may be a susceptibility factor for infection). Kim et al. [19] found that there was no difference in prednisolone alone or prednisolone plus adjuvant with regard to prognosis and time to remission in PV patients [19].
Most bacterial skin infections detected in our patients were due to Staphylococcus aureus. In other studies, in PV patients, skin infections due to Staphylococcus aureus have been reported as well [20]. In the study by Kanwar and Dhar, among the causes of 10 deaths of PV, sepsis was the most common cause and the responsible pathogenic agent in 4 cases was Staphylococcus aureus [21]. Escherichia coli were the most frequent cause ofurinary tract infection in our study. Obviously, Escherichia coli is the most common cause of urinary tract infections in the general population [22].
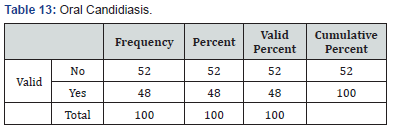
In the current study, 9.68% of patients had localized herpes simplex infection; while in the study of Belgnaoui et al. [6] 17% of patients had localized herpes infection [6]. In several reports, the herpes infection has been studied in PV patients [6,23,24]. Although high doses of corticosteroid and immunosuppressive therapy would cause patients to be prone to an extensive herpes simplex virus infection, in this study, we had only localized herpes simplex virus infections [24]. Previously, our group had studied the herpes simplex infection and PV in Iranian patients [10]. In that study we concluded that a herpes virus infection occasionally is responsible for exacerbation of PV [10]. In the current study, 23.87% of patients had oral candidiasis (Table 13), while in the study of Belgnaoui et al. [25] 30% of patients had oral candidiasis [6]. With regard to oral candidiasis, the result of the two studies is similar. Previously, laryngeal candidiasis has been reported in patients with PV, but in this study we had only localized oral candidiasis [25].
Infection rate had a positive significant relationship with the number of admission sessions. Patients with multiple admission sessions had a rate of infection approximately two times more than patients admitted for first time. Logically, patients with a more severe disease would have more admissions, and consequently the rate of infections would increase. Retrospective nature and relatively short period of the study (2 years) are major limitations of this project. Another limitation of the study is PV patients on different immunosuppressive adjuvant therapy included in this study. A prospective study with follow-up is recommended. We concluded that PV patients with multiple admission sessions, diabetes mellitus, and severe disease are at higher risk of infection. According to a high rate of antimicrobial resistance, antibiograms are recommended for antibiotics therapy (Table 14).
For more Open Access Journals
in Juniper Publishers please click on: https://juniperpublishers.com/
For more details JOJ Dermatology & Cosmetics (JOJDC) please
click on: https://juniperpublishers.com/jojdc/index.php

Comments
Post a Comment