Treatment of the Ear Giant Keratoacanthoma with Topical Imiquimod-Juniper Publishers
Authored
by Hong-Duo Chen

Abstract
Keratoacanthoma (KA) is an epidermal neoplasma with
rapid growth and severe local destruction. Owing to its similarities to
squamous cell carcinoma, complete surgical excision is mainly
recommended. Topical imiquimod is an ideal option for the problematic
sites and cosmetic demands. Here we report a giant case of KA on a rare
anatomical location, and fully recorded the disease process. The patient
was treated successfully with topical imiquimod.
Keywords: Keratoacanthoma; Imiquimod
What’s already known about this topic?
Keratoacanthoma (KA) is an epidermal neoplasma with
rapid growth and local destruction. Topical imiquimod is an ideal option
for the problematic sites and cosmetic demands.
What does this study add?
• The patient presented with a giant KA lesions on
the left anthelix, which was a rare anatomical location and not recorded
in the medical literatures.
• The tumor process was fully described in our study.
• The tumor was successfully treated with topical
imiquimod, which provides a valuable reference for the treatment of some
malignant skin tumors with the topical immune regulatory therapy
Introduction
Keratoacanthoma (KA) is an epidermal neoplasma with
rapid growth and spontaneous regression tendency. Owing to its
similarities to squamous cell carcinoma (SCC) and severe local
destruction, complete surgical excision is mainly recommended. However,
nonsurgical options are required in consideration of the tumor size,
problematic sites, and cosmetic demands [1,2]. Here, we report a giant
KA case on the rare location successfully treated with topical
imiquimod.
Case Report
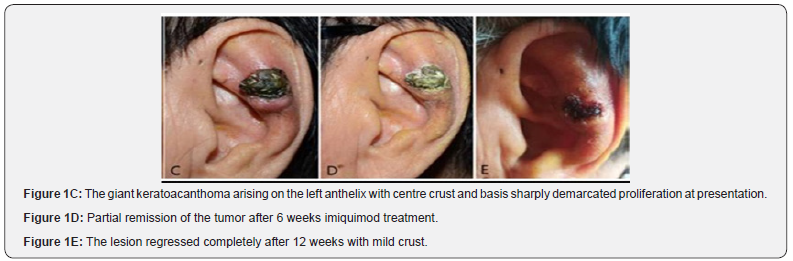
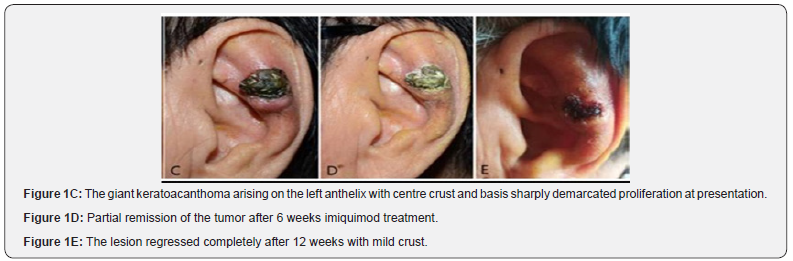
A 87-year-old Chinese man presented to our clinic
with rapidly growing large ear tumor for 6 months duration. The skin
examination revealed a well-circumscribed, measuring about 3×3cm,
black-crusted crateriform tumor on the left ear. The lesion started as
little papule with centre keratin plug suspect as virus wart, no
treatment was given. The tumor rapidly grew to 3cm in diameter; and the
centre crust and ulceration with basis proliferation were observed at
presentation (Figure1 A-D).

The previous history included prostate cancer and colon tumor with
surgery treatment. Lab assay revealed mild decreased hemoglobins;
hepatorenal functions were within normal limits. No enlarged
superficial lymph node was palpable. Head-neck and thoracic computer
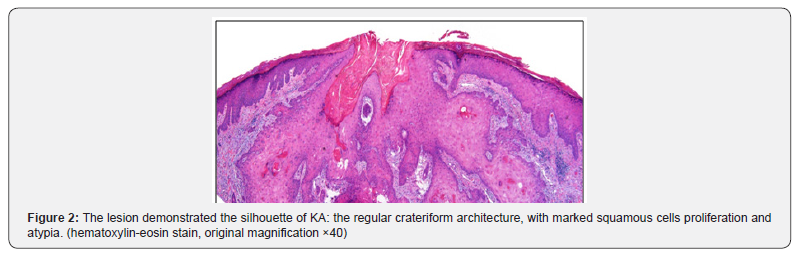
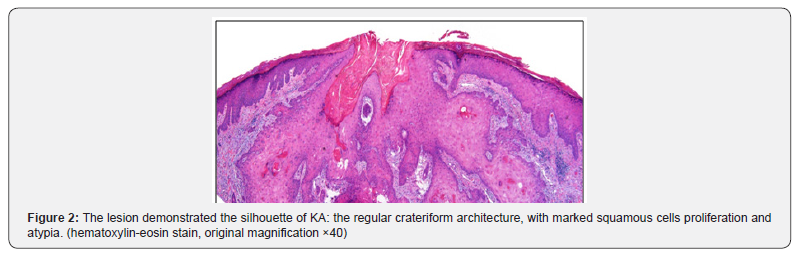
tomography were carried out with negative results. Histopathological
examination exhibited the regular crateriform architecture, with marked
hyperkeratosis, acanthosis and papillomatosis; the atypia of squamous
cells were found (Figure 2). The diagnosis of KA was confirmed. We
treated him with the imiquimod cream once every 2 days. The tumor
remarkably decreased in size after 6 week treatment. After 12 weeks, the
lesion was almost completely cleared leaving mild crust. (Figure1E-F)
Maintained treatment was applied for another 4 weeks.
Discussion
Keratoacanthoma (KA) is a benign epidermal neoplasma with
local destruction. The aetiopathogenesis still remains uncertain. The
complete process of the disease commonly lasts 4-9 months [2] KA
is generally considered relevance to previous skin trauma, such as
laser treatment and scars, and probably having relations to systemic
immunosuppressive therapy [3-5]. Since the histological features of KA
bears a close resemblance to typical SCC, and no befitting criterion can
be used to distinguish with sufficient sensitivity and specificity, complete
surgical excision was usually nominated for most cases [6]. However,
surgery approach has its limitations. KA commonly grows on face and
neck, oversized tumor and the problematic sites pose special difficulties
for complete excision considering the cosmetic and functional need.
When underlying malignancies have to be taken into account, alternative
therapies are broadly researched all along.
A research indicated that topical imiquimod cream, topical
5-fluorouracil, intralesional 5FU, intralesional methotrexate,
intralesional bleomycin, and intralesional interferon all showed high
clearance rates when applied in KA [1] Among them topical imiquimod
(once daily, 3 to 4 days per week, 12 weeks duration) even showed 100%
clearance rate in the treatment of KA. Previous reports proved the same
curative effects while applying topical imiquimod to KA lesions with the
usage above [7,8]. Imiquimod, known as an immune-response modifier,
can interact with Toll-like receptor 7 on antigen-presenting dendritic
cells. After activating both the innate and acquired immune systems with
the expression of varieties of cytokines, it can subsequently destruct
tumor cells [9]. Along with therapeutic process, side effect as restricted
severe inflammatory reactions seems unavoidable [7-10]. In our case,
the tumor was located at the left anthelix, which was rare in previous
reports. Considering the problematic anatomical location and tumor
size, topical imiquimod was given. After about 12-week treatment, the
tumor was cleared. Another 4 weeks maintained treatment was given for
the high risk of malignancy.
In summary, we report and add to the medical literature a unique
case of giant keratoacanthoma of anthelix with fully recorded disease
process, which was successfully treated with topical imiquimod. Our
research provides a valuable reference for the treatment of some
malignant skin tumors with the immunoregulatory therapy of topical
imqumoid.
For more
details JOJ Dermatology & Cosmetics
(JOJDC) please
click on: https://juniperpublishers.com/jojdc/classification.php

Comments
Post a Comment