Improvement in Scalp Dermatomyositis with Platelet-Rich Plasma-Juniper Publishers
Authored
by Hosking AM
Abstract
Dermatomyositis (DM) is an inflammatory myopathy with
hallmark cutaneous findings, including heliotrope rash, Gottron’s
papules, as well as photodistributed erythema and/or poikiloderma. Scalp
DM (SDM) presents as erythematous plaques with overlying scale,
associated with severe burning pruritus. Due to inflammation, it may
also present with non-scarring alopecia. First-line treatment for SDM
includes intralesional corticosteroids; however, to date, no therapy has
proven effective. Platelet-rich plasma (PRP) is an emerging treatment
modality for a variety of disease entities including arthritis, oral
surgery, and skin rejuvenation. Recent reports demonstrate PRP may have a
promising role in hair regrowth. Herein, we report a case of refractory
SDM with significant clinical improvement after treatment with
subdermal PRP injections of the scalp. We also used optical coherence
tomography (OCT) as a non-invasive imaging methodology to longitudinally
monitor hair growth over the 18-week PRP treatment interval.
Keywords: Dermatomyositis; Scalp; Platelet-rich plasma; Tomography
Abbrevations: DM: Dermatomyositis; OCT: Optical Coherence Tomography; PRP: Platelet-Rich Plasma; SDM: Scalp DM
Introduction
Dermatomyositis (DM) is a systemic, autoimmune,
connective tissue disease characterized by chronic muscle inflammation
and weakness associated with characteristic cutaneous findings. The
disease predominantly affects females compared to males (2:1) and may be
associated with occult malignancy [1]. Scalp dermatomyositis (SDM) is
seen in 28-82% of patients with dermatomyositis, and presents with
diffuse erythema, scale, and poikiloderma of the scalp, with associated
non-scarring alopecia [2,3]. Severe, debilitating, burning pruritus is a
common symptom, and can help differentiate SDM from other autoimmune
causes of hair loss, including lupus and scleroderma [4]. Treatment
options include intralesional triamcinolone, as well as systemic
corticosteroids, immunomodulators and immunosuppressants to treat the
underlying disease. However, SDM is often treatment-resistant, and the
above therapies are limited by efficacy, adverse events, and disease
recurrence after treatment cessation.
Platelet-rich plasma (PRP) has been used for many
years in orthopedics, plastic surgery, and maxillofacial surgery. PRP
has recently attracted attention in the field of dermatology for its
ability to promote tissue regeneration, wound healing, and
potential to stimulate hair growth. PRP consists of the fraction of
blood plasma with a higher concentration of platelets (generally two to
five-fold higher than baseline) and has been shown to activate human
dermal fibroblast proliferation, as well as increase type 1 collagen
synthesis [5,6]. Studies have demonstrated an anti-inflammatory effect
of PRP, with platelet activation leading to release of inflammatory
mediators. Specifically, anti-inflammatory cytokines, such as IL-4 and
IL-10, are significantly upregulated in comparison to pro-inflammatory
cytokines, such as IL-1β [7]. Herein, we report a case of SDM with
significant clinical improvement after treatment with subdermal PRP
scalp injections.
Case Report
A 35-year-old, Asian female with a 12-year history
of dermatomyositis presents for evaluation of alopecia and scalp
dermatitis and pruritus consistent with SDM. For treatment of systemic
disease, she has been receiving monthly intravenous immunoglobulin
(IVIg) infusions for 11 years, with significant improvement in myalgia
and muscle weakness; however, she continues to experience persistent,
relapsing alopecia and intractable pruritus with scalp thickening and
lichenification.
For SDM, the patient was previously treated with intralesional
triamcinolone, T/Gel® shampoo, ketoconazole 2% shampoo,
topical clobetasol 0.05%, topical calcipotriene 0.005%, topical
betamethasone dipropionate 0.064%, and a four-week course
of excimer laser, all without significant clinical improvement.
The patient’s only current treatment regimen includes monthly
intralesional triamcinolone (5mg/mL) injections for the past two
years, which have been moderately successful at relieving her
symptoms and poorly controlling SDM clinical progression.
Physical examination reveals a well-appearing female with
Fitzpatrick type 3 skin with scattered, erythematous, thin plaques
with scale over the neck and shoulders, violaceous papules
over the extensor aspects of the metacarpophalangeal and
interphalangeal joints (Gottron papules) with interphalangeal
involvement, ragged cuticles, and trace swelling of all digits. The
shawl sign is present with erythema and fine papules with scale
over the lateral and posterior neck, as well as the décolletage.
She also has faint violaceous patches covering the upper eyelids,
consistent with a mild helitrope rash. Examination of the scalp
demonstrates diffuse hair thinning with patch-like distribution,
atrophic erythematous plaques with hyperkeratotic scale and
lichenification, and scattered hyper- and hypopigmented atrophic
plaques at the temporal and occipital hairlines. Her eyelashes
appear normal; however, there is thinning of bilateral, lateral
eyebrows.
In addition to her intralesional corticosteroid injections, we
performed three sessions of subdermal injections of PRP (Eclipse
Aesthetics, LLC, The Colony, TX, USA) in the scalp over 18 weeks,
with an average of 9mL of PRP injected each session. The PRP
sample was obtained after centrifuging 22mL of whole blood
and extracting the platelet-rich fraction per company protocol.
Three weeks after receiving her first session of PRP, there was
significant improvement in epidermal thickness, scale, bogginess,
and erythema. The patient reported improvement in pruritus and
burning sensation as well as decreased shedding.
The patient continued her remarkable improvement after the
second session of PRP. However, shortly before her third session
the patient experienced a mild flare, with increased pruritus and
accompanied by systemic fatigue. Six weeks after her last PRP
treatment, the patient appeared “much improved” compared to
baseline on a Global Impression of Improvement of Alopecia Scale
(from “worse” to “very much improved”) as rated by both patient
and physician, and reported persistent, but improved, pruritus
and scale over the scalp (Figure 1). The patient was subsequently
started on oral plaquenil per rheumatology in an effort to better
control systemic disease.

In addition to the above subjective measures, we also used
a novel, non-invasive imaging system called optical coherence
tomography (OCT) to quantitatively follow our patient’s clinical
progress. OCT uses low-coherence interferometry to measure
the back-scatter of broad-bandwidth light, producing sub-surface
images of the scalp at a depth of approximately 1300 to 1500μm
with a resolution of 10μm [8]. This imaging technique may be used
to provide quantitative information on hair follicle density and can
be used to longitudinally follow the clinical progress of alopecia
patients in the outpatient clinical setting.
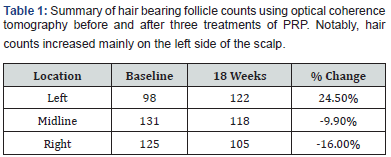
We used OCT to measure nine different scalp locations,
including the frontal hairline, temporal regions, crown and vertex,
using a 5mm x 7mm scanning window (Table 1). Although both
the investigator and the patient subjectively reported global
improvement in hair loss, OCT data was not consistent with these
findings. OCT demonstrates increased active hair follicle count on
the left parietal (24.5%) with loss in the midline (-9.9%) and on
the right (-16.0%). This conflicting data may be consistent with
SDM disease course reflecting improvements and flares in disease
activity resulting in hair loss in specific scalp areas. Although PRP
may improve symptoms of SDM, it does not necessarily induce
stable hair regrowth.
Discussion
Involvement of the scalp is a common clinical finding in
DM, with one case series reporting scalp involvement in 77.4%
patients and alopecia in 87.5% [2]. In the largest histopathologic
study of SDM biopsy specimens to date (n=36 specimens from
20 patients), SDM demonstrates interface dermatitis, thickening
of the basement membrane, preserved follicular architecture,
telangiectasia, and mucin deposition. On horizontal sections, hair
counts were most consistent with a diagnosis of chronic telogen
effluvium [2]. On trichoscopy, SDM shows enlarged tortuous
capillaries, peripilar casts, tufting, and interfollicular scaling.
Serologic abnormalities associated with DM include anti-Jo,
anti-Ku, and anti-MDA-5 antibodies. The anti-MDA-5 antibody is
associated with increased risk of SDM and alopecia [9]. It is possible
that in some patients, SDM may be the initial presentation of DM,
with the scaly dermatitis often misdiagnosed as sebopsoriasis or
seborrheic dermatitis [10].
Systemic treatment of DM often results in a discordance
between the response seen in muscle disease and cutaneous
disease [11]. Even with remission of muscular disease, cutaneous
involvement often persists. Treatment for cutaneous DM may
include sun protection, topical or intralesional corticosteroids,
topical corticosteroid-sparing agents, such as calcineurininhibitors
or retinoid, and/or systemic therapies, such as
hydroxychloroquine or low-dose, weekly methotrexate [11]. SDM
is particularly challenging to treat and often persists with systemic
treatment despite resolution of other cutaneous involvement [12].
Although the mechanism for improvement of SDM’s clinical
signs and symptoms with PRP is unknown, the authors feel this
topic warrants further investigation. In chronic wound healing,
PRP promotes new capillary growth and stimulates epithelization
[13]. In orthopedic injuries, PRP has been shown to suppress
cytokine release and decrease inflammation, thereby promoting
tissue healing [13,14]. We hypothesize that PRP may help
attenuate the inflammatory response seen in cutaneous and scalp
DM, thus promoting lesion healing. In our experience, autologous
PRP injection in the scalp carries little risk with bruising and scalp
tenderness being the most commonly reported adverse events. In
the literature, rare reports of infection and nerve damage exist,
and there is one case of blindness resulting from periocular PRP
injections for skin rejuvenation [15]. PRP of the scalp may offer a
low-risk complementary or alternative treatment to conventional
DM therapy, especially in the case of recalcitrant scalp disease.
Conclusion
SDM can be a debilitating manifestation of DM. Often,
conventional therapies do not offer patients relief from the clinical
signs and symptoms of disease and are accompanied by unwanted
adverse events and disease recurrence after treatment cessation.
As evidenced by this case, PRP may be a promising treatment
modality for SDM by decreasing inflammation in the scalp and
providing transient improvement of clinical signs and symptoms
of disease; however, the use of PRP may not necessarily result in
hair growth in highly inflammatory scalp conditions.
For more
details JOJ Dermatology & Cosmetics
(JOJDC) please
click on: https://juniperpublishers.com/jojdc/classification.php
To read more…Full Text
in Juniper Publishers click on https://juniperpublishers.com/jojdc/JOJDC.MS.ID.555562.php

Comments
Post a Comment